Immune Thrombocytopenic Purpura (ITP) is a condition where the body's immune system mistakenly attacks and destroys its own blood clotting cells called platelets. This can lead to easy bruising and bleeding.
There are two types of ITP:
ITP is also classified based on the duration of the condition:
Immune thrombocytopenia (ITP) disease can present with a wide range of symptoms or, in some cases, no symptoms at all, making it difficult to diagnose.
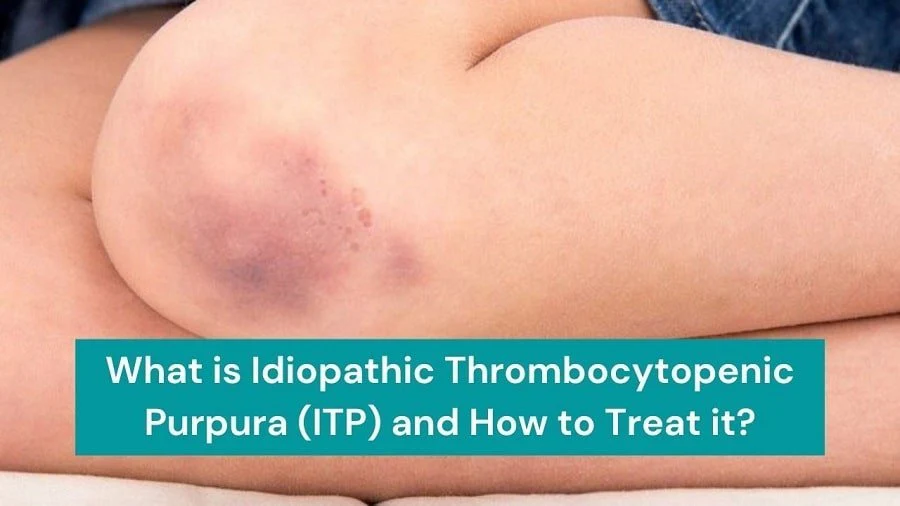
ITP can lead to easy bruising, even with minor injuries. This occurs because a reduced platelet count impairs the blood's ability to form clots effectively.
One symptom of ITP is the presence of tiny reddish-purple spots in the skin, known as petechiae. These spots are most commonly seen on the lower legs and can resemble a rash. They develop due to minor blood vessels bleeding under the skin.
In more severe cases, people may notice larger areas of bleeding into the skin, referred to as purpura. Purpura typically appears as more significant, dark patches on the skin caused by increased blood vessel leakage.
People with ITP may experience bleeding from the gums or nose, often with no apparent cause. A low platelet count can compromise the blood vessels' ability to withstand even minor trauma.
In some instances, ITP can lead to blood appearing in urine or stools. This symptom should be taken seriously, and immediate medical attention is necessary to determine the underlying cause.
For female patients with ITP, a hefty menstrual flow can be a noticeable symptom. The reduced platelet count can affect the blood's clotting ability during menstruation, leading to heavier bleeding.
ITP, or Immune Thrombocytopenia, is a non-contagious blood disorder. It cannot be transmitted from one person to another. This condition can be categorised as primary, occurring independently, or secondary, triggered by other underlying conditions.
Possible triggers for secondary ITP include:
ITP is often called "idiopathic," meaning it has no known cause. This is because the condition is not hereditary, and there is no apparent predisposition for primary ITP.
Diagnosing Idiopathic Thrombocytopenic Purpura (ITP) involves a few steps because there isn't a specific test that can definitively diagnose the condition. Instead, doctors use a combination of medical history, physical examination, and lab tests to diagnose.
This test is more common in adults than in children. A small sample of bone marrow (the spongy tissue inside bones where blood cells are made) is taken and examined to rule out other diseases that might be causing low platelet counts.
The treatment choice for ITP is based on several factors, including the patient's platelet count, the frequency and severity of bleeding, and individual characteristics. Here's a summary of the treatment options mentioned:
In some cases, especially with mild or acute ITP in children, treatment may not be necessary as the condition can improve on its own.
If treatment is required, medications are often the first line of therapy. The following medications may be used:
In cases of severe ITP that do not respond to medications or other treatments, a splenectomy may be considered. A splenectomy involves the surgical removal of the spleen. The spleen is where platelets can be sequestered and destroyed, so removing it can help increase platelet counts. However, this procedure is usually reserved for adults with severe ITP as children often experience spontaneous remission, and splenectomy can increase the risk of certain bacterial infections in the future.
Severe or widespread ITP can be a medical emergency due to the risk of life-threatening bleeding. Emergency treatments may include transfusions of concentrated platelets and the intravenous administration of corticosteroids (e.g., methylprednisolone), IVIg, or anti-D treatments to increase platelet counts and control bleeding rapidly.
Patients with ITP may be advised to make certain lifestyle modifications to ease the risk of bleeding and improve their overall health. These changes may include:
Treatment for women with ITP during pregnancy depends on their platelet count. Those with mild ITP cases typically require no treatment apart from vigilant monitoring and routine blood tests.
However, for women with an exceedingly low platelet count late in pregnancy, there is an elevated risk of substantial and severe bleeding during and after childbirth. In such instances, the attending physician will collaborate with the women to establish a treatment strategy aimed at sustaining a safe platelet count while safeguarding the well-being of the baby.
Women who experience ITP concurrently with other significant pregnancy-related conditions, such as preeclampsia, will require treatment as well.
While the majority of infants born to mothers with ITP are unaffected by the disorder, some may be born with or develop a low platelet count shortly after birth. Babies with severely diminished platelet counts may necessitate treatment.
we offer personalised care and advanced treatments for immune thrombocytopenia (ITP). Our diagnosis process includes a medical history review and blood tests. Treatment options range from medication and antibody therapy to splenectomy in severe cases. In emergencies, our swift and effective care is your solution. We also guide lifestyle changes and tailored pregnancy management. Your well-being is our top priority.
© 2026, Dr Krishna Kant Singh. All Rights Reserved.